Day 46 (of 2024/25) Epilepsy Training update re BC Epilepsy Society
Great opportunity to update some knowledge about epilepsy! Things have changed over the years in schools… less 1:1 support ‘just in case’ and more knowledge and understanding about epilepsy…
- Facts about epilepsy and seizures
- Main types of seizures
- First aid and safety considerations
- Understanding learning and behavioural considerations
- What is epilepsy
- Sudden, brief and temporary disturbance of electrical activity in our brain
- Can result in a change of behaviours/body actions
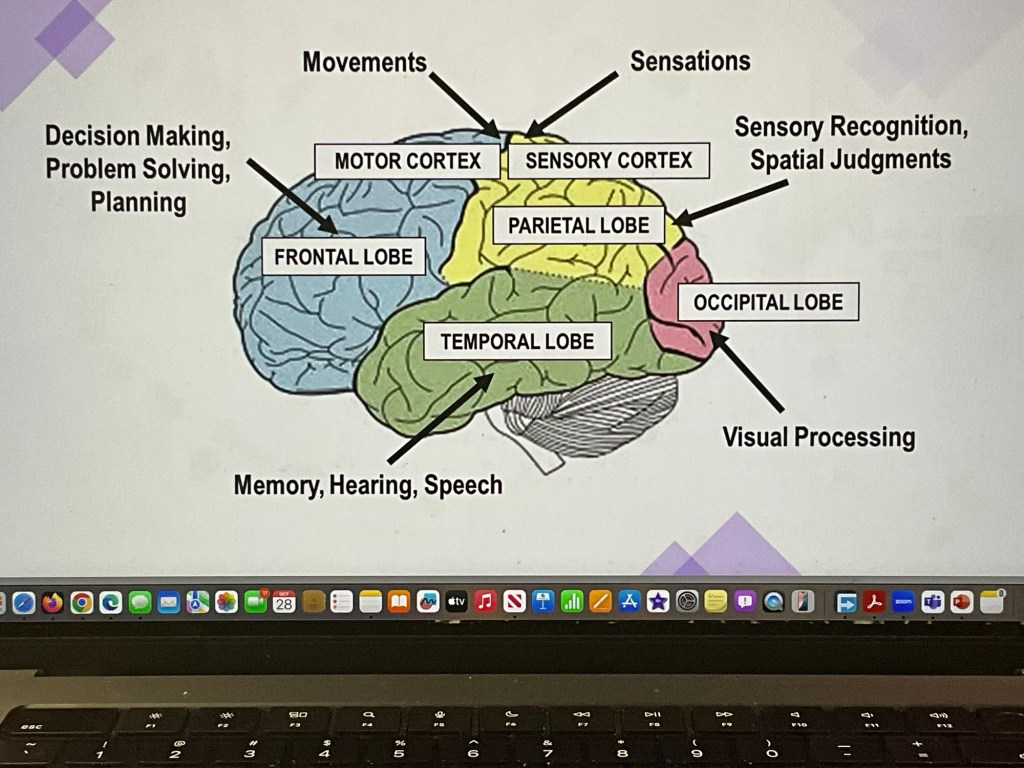
- Symptoms depend on brain area
- Seizure does not mean you have epilepsy (fever, toxic reaction, irregular heartbeat, low blood sugar, lack of oxygen, functional (psychogenic) seizure
- 1 in 10 will experience a seizure; 1 in 100 will develop epilepsy; 50 000 in BC; 65 million+ in world; across all demographics; including in people with cerebral palsy, autism, Down’s syndrome, FAS, tuberous sclerosis (rare – tumours on organs)
- Coexist with depression, anxiety, adhd, migraines <— often linked for a reason for ‘greater than average chance’ – though not necessarily always with each other <— not a risk factor for epilepsy
- Can come across as a panic attack/anxiety disorder – and a biological response; an anxiety related seizure; feelings can well up without stimuli – and can also be very short in time…
Spectrum of severity
Uncomplicated <——> Complicated
Controlled <——> intractable (eg on 5 medications but still not predictable… things are still not working)
30% of people with epilepsy do not have their seizures completely controlled <— drug resistant epilepsy – sometimes brain surgery works, but not always…
What causes epilepsy?
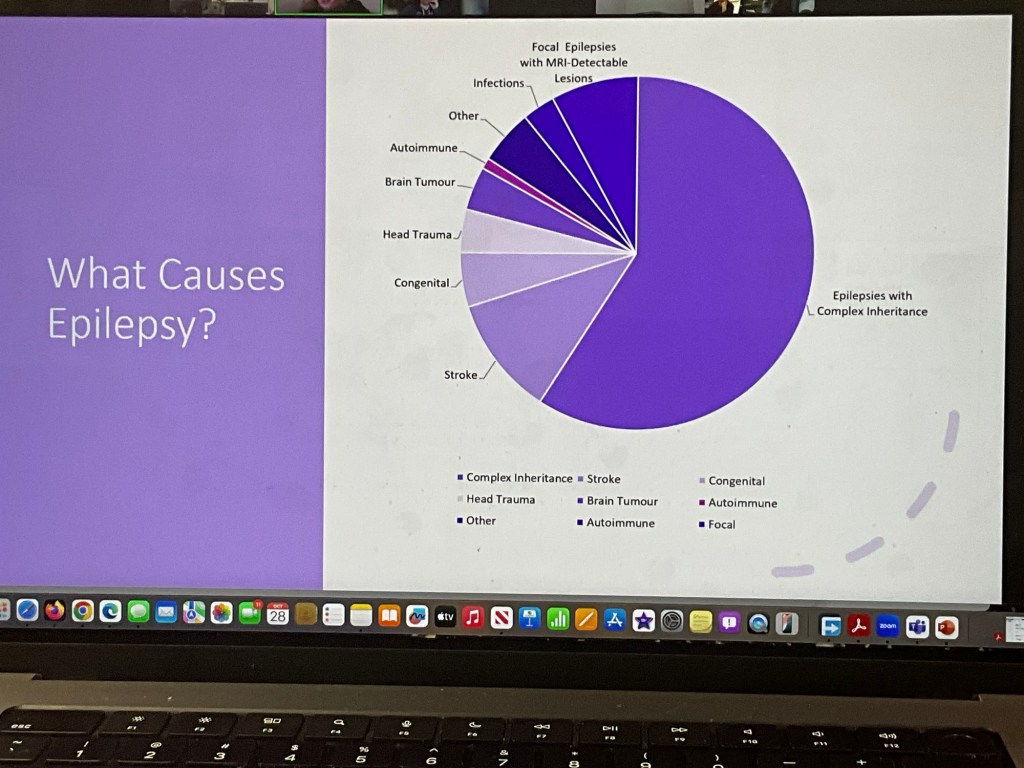
Genetics take on the biggest role – not necessarily what was inherited directly from one parent… but how the genes react and interrelate with the environment
How Treated:
- Medications
- Neuro stimulation with Devices
- Dietary Therapy
- Epilepsy Brain Surgery
Types of seizures
Generalized: all over the brain
Focal: specific location
Absence seizure –
- blackout; brief loss of awareness; loss of consciousness; may be eyelid fluttering or lip chewing; returns to full awareness almost immediately; no recollection of missed time; may occur multiple times a day
- often confused with daydreaming and attention problems –
- length: usually less than 20 seconds.
Ie – student often great with answers, sometimes nonsense answers – turns out had minor seizures and gave quick responses to avoid embarrassment of having no answers.
Tonic-Clonic Seizure
- usually lasts 1-3 minutes
- Loss of consciousness; stiffening of body (tonic); convulsions (clonic); shallow breathing; sound – oxygen coming out; possible loss of bladder; drooling; skin may turn blue;
- followed by confusion, headache, tired, sore, difficulty talking
Myoclonic Seizure
- person remains conscious
- Brief jerk or seizure
- Unusually involves the neck, shoulders and arms
- Can be aware – and can get frustrated
Focal Aware Seizure
- person is fully aware
- No loss of consciousness
- Senses are distorted
- Rhythmic twitching or jerking
- Sensory symptoms
- Voices… burnt toast… hallucinations… (Brain complicated – symptoms can be same as other brain related issues)
- Other symptoms (fear, anxiety, deja vu)
- Often confused with: psychosomatic illness, mystical experience
- Usually last less than 1 minute
Focal Impaired Awareness Seizure
- awareness is impaired
- May be confused/unable to respond
- May being blank/dazed
- not in control of movement, speech or actions
- Automatisms – purposeless respective actions
- Clumsy or disoriented
- May not be able to talk etc
- Not aware (eg take of clothes in public; act aggressive – touching someone) but socially in appropriate
- Short time frame as well
Postictal (recovery phase)
- time after – needs to be safe space with safe person
How do we know seizure is over: jerking ends; person seems okay, but brain may not be fully ‘rebooted’ yet; wait until they ask: what happened? Where am I?
Those who know the person will know when the brain has rebooted based on patterns.
It is possible to have a seizure pattern
BIG questions
Don’t ask yes/now questions; what is your moms name…
How long? 20 minutes post-seizure
Warning before a seizure? Occasionally an ‘aura’ – focal seizure – these need to be tracked because they can progress to a more severe seizure… (big seizure won’t always happy)
What triggers:
Missed medication #1
Sleep Deprivation # 2
Flickering lights (famous but low frequency)
More personalized:
Severe stress
Illness or fever
Hormonal changes
Drug interactions
Alcohol and or drug use
Hyperventilation
Dehydration
Overheating
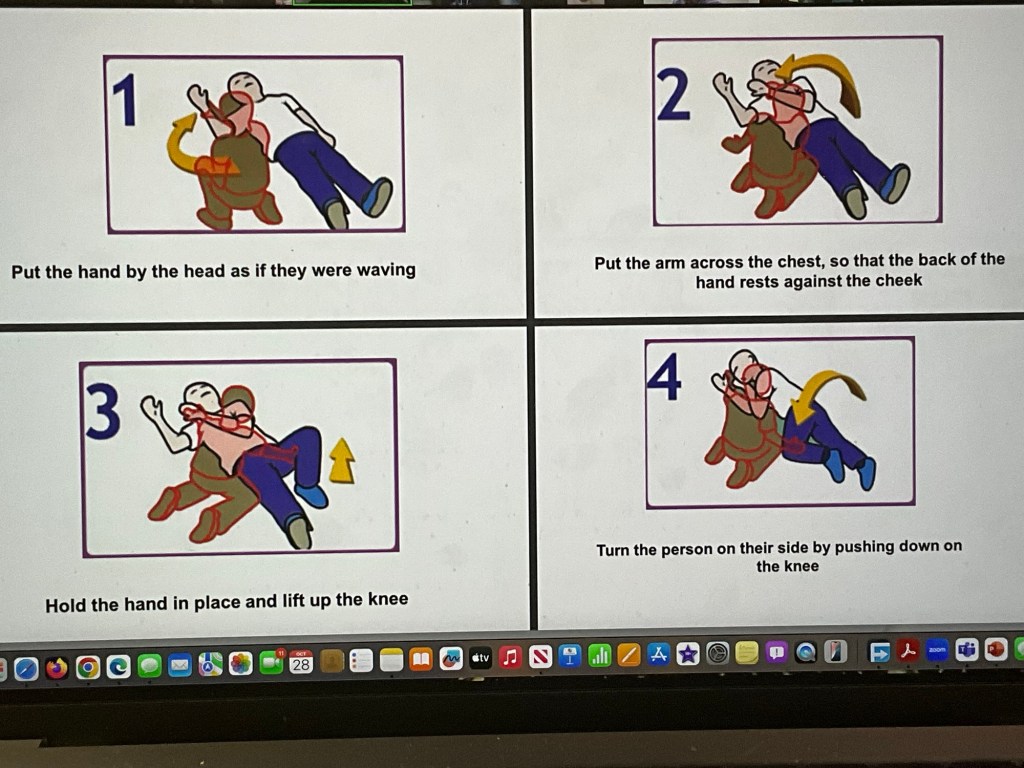
Seizure First Aid:
- Stay Calm
- Time the Seizure
- Protect from Injury
- Cushion head
- Move hard or sharp objects away
- Gently guide away from hazards
- Loosen any tight clothing around the neck
Seizures are normal… even though for many it feels very unnormal.. 99.5% of the time the person will be fine.
- Turn them on their side
- Stay with them
- Be reassuring and comforting
- Document seizure activity (what happened before; during and after the seizure)
WHAT NOT TO DO:
DO NOT:
- put something in a persons mouth
- Hold down/restrain them
- Give food or drink
- Keep them on their back
- Leave a person; call for help
- Film someone’s seizure
There are times to call 911
- usually after 5 minutes
- first time seizure
- Seizures repeat without body relaxing
- Confusion persists for more than 20 minutes *unless you know the persons seizure history goes beyond 20 minutes
- Difficulty breathing
- Occurs in the water
- Individual is injured, has diabetes, or is pregnant
In wheelchair?
- lock wheels
- Secure wheelchair
- Fasten seatbelt
- Protect/support the head
- Make sure breathing is not blocked
On Bus
- pull over and stop the bus
- Place student on their side across the seat
- Remind others to stay in their seats
Seizure Action Plan (needed with rescue meds)
What to record:
- time (start and finish)
- Warning signs
- Movements and actions
- Muscle tone
- Change in skin colour
Not everything is epilepsy related
Confidence and motivation may be diminished by societal attitudes and expectation
But…
- problems with attention and memory
- Fatigue/sleepiness
- Anxiety/depression
- Overprotection
- Learned helplessness
- Social isolation
- Low self esteem
- Stigmatization
Teaching strategies:
- access to alternative, quiet work areas
- Repetition and rehearsal
- Mini size distractions
- Structure of the classroom and lessons
- Break down assignments
- Extended time for assignments and tests
Tips:
- stay calm and reassuring
- Treat each student as an individual
- Avoid overprotection and encourage independence
- Don’t talk about student like they aren’t there
- Facilitate positive peer interactions and inclusions
- Don’t let the focus be on the student’s conditions
Reminder:
Hard to be a parent (as it is) with a child who has seizures.
Hard to be a kid with so many adults ‘watching like a hawk’…
- sometimes need to be watched… you go unconscious, so presenter shared she would literally ‘walk into traffic’ because had moments of complete unawareness… balancing overprotection and learned helplessness and independence
There is community – especially for newly diagnosed
BC Epilepsy Society: http://www.bcepilepsy.com
The more we know…
Leave a comment